buy cough syrup, Uncategorized
Valium Withdrawals | Symptoms, Timeline & Safe Diazepam
Valium Withdrawals | Symptoms, Timeline & Safe Diazepam Withdrawal Treatments
Valium withdrawals can be overwhelming and potentially dangerous without proper medical guidance. If you’re currently taking Valium (diazepam) and considering stopping, or if you’ve already begun experiencing withdrawal symptoms, this guide is for you.
Whether you’ve been prescribed Valium for anxiety, muscle spasms, or seizures, stopping this benzodiazepine requires careful planning. Many people don’t realize that even when taken as prescribed, Valium can lead to physical dependence, making sudden discontinuation risky.
This article covers everything you need to know about safely navigating diazepam withdrawal. We’ll walk you through the complete Valium withdrawal timeline so you know what to expect during each phase of recovery. You’ll also learn about safe medical detox and tapering strategies that can minimize uncomfortable symptoms while protecting your health. Finally, we’ll explore natural support methods and long-term recovery approaches to help you build a foundation for lasting success.
If you’re ready to break free from Valium dependence, understanding the withdrawal process is your first step toward recovery.
Understanding Valium and Its Effects on Your Body
What Valium Is and How It Works in Your Brain
Valium, known generically as diazepam, belongs to a class of medications called benzodiazepines. This powerful sedative works by enhancing the effects of GABA (gamma-aminobutyric acid), your brain’s primary inhibitory neurotransmitter. Think of GABA as your brain’s natural brake system – it slows down neural activity and promotes feelings of calm and relaxation.
When you take Valium, it binds to specific receptors in your brain called GABA-A receptors. This binding dramatically amplifies GABA’s calming effects, which is why Valium can quickly reduce anxiety, muscle tension, and even stop seizures. The medication essentially floods your nervous system with artificial tranquility, creating the sedating and anti-anxiety effects people seek.
Doctors commonly prescribe Valium for anxiety disorders, panic attacks, muscle spasms, and alcohol withdrawal symptoms. Its long half-life means it stays in your system much longer than other benzodiazepines – sometimes up to 200 hours depending on various factors like age, liver function, and overall health.
Why Your Body Becomes Dependent on Diazepam
Your brain adapts remarkably quickly to Valium’s presence. Within weeks of regular use, your natural GABA production begins to decrease because your brain assumes the medication will handle the job instead. This process, called neuroadaptation, happens automatically as your body tries to maintain balance.
Benzodiazepine tolerance develops as your brain creates more GABA receptors to compensate for the constant artificial stimulation. What once felt like adequate relief from one pill now requires two, then three, creating a dangerous cycle. Your nervous system essentially rewires itself around Valium’s presence.
Physical dependence can occur even when taking Valium exactly as prescribed by your doctor. Many people discover their dependence only when they try to stop or miss a dose, experiencing uncomfortable symptoms like rebound anxiety, insomnia, or physical discomfort. This isn’t a sign of weakness or moral failing – it’s a predictable biological response to prolonged benzodiazepine exposure.
The longer you take Valium and the higher your dose, the more entrenched this dependence becomes. Your brain forgets how to regulate anxiety and relaxation naturally, making discontinuation challenging without proper medical support.
The Difference Between Physical Dependence and Addiction
Physical dependence and Valium addiction represent two distinct but often confused conditions. Physical dependence is a biological state where your body needs the medication to function normally. You can be physically dependent on Valium while taking it responsibly under medical supervision.
Addiction, however, involves compulsive drug-seeking behavior despite negative consequences. Someone with Valium addiction might doctor shop for multiple prescriptions, take higher doses than prescribed, or continue using despite relationship problems, work issues, or health complications.
Many people develop physical dependence without addiction. They take their prescribed dose consistently, don’t crave extra pills, and want to stop but fear withdrawal symptoms. These individuals need medical tapering support but don’t necessarily require addiction treatment programs.
| Physical Dependence | Addiction |
|---|---|
| Predictable biological response | Compulsive behavior patterns |
| Can occur with prescribed use | Involves drug-seeking behaviors |
| Withdrawal symptoms when stopping | Continued use despite harm |
| Managed through medical tapering | Requires comprehensive treatment |
| No loss of control over use | Loss of control over consumption |
Recognizing this difference helps people seek appropriate treatment. Someone with pure physical dependence might need gradual dose reduction and withdrawal support, while addiction typically requires psychological interventions, counseling, and long-term recovery planning.
Both conditions deserve medical attention and compassionate care. Neither reflects personal weakness – they’re medical conditions requiring professional treatment approaches tailored to individual needs and circumstances.
Recognizing Valium Withdrawal Symptoms
Physical Symptoms That Signal Withdrawal
The body’s response to stopping or reducing Valium can be intense and uncomfortable. Physical withdrawal from Valium typically begins within 6-24 hours after your last dose, as diazepam leaves your system. Your nervous system, which has become dependent on the drug’s calming effects, starts to rebel without its usual chemical support.
Tremors and muscle tension are among the first signs you’ll notice. Your hands might shake when reaching for a cup of coffee, or your shoulders could feel like they’re carrying invisible weight. Sleep becomes elusive – you might find yourself lying awake despite feeling exhausted, or waking up drenched in sweat multiple times per night.
Headaches often accompany early withdrawal, ranging from dull pressure to sharp, throbbing pain. Your digestive system may also revolt with nausea, vomiting, or loss of appetite. Many people experience heightened sensitivity to light and sound, making everyday environments feel overwhelming.
Common Physical Symptoms:
Muscle aches and stiffness
Rapid heartbeat or palpitations
Excessive sweating
Dizziness or lightheadedness
Blurred vision
Stomach cramps and digestive issues
Fatigue combined with restlessness
These symptoms reflect your GABA neurotransmitter system struggling to regain balance without Valium’s artificial enhancement.
Emotional and Mental Health Changes During Withdrawal
Psychological withdrawal from Valium can feel like an emotional rollercoaster that never stops. Your brain chemistry has adapted to function with the drug’s presence, and removing it leaves you vulnerable to intense mood swings and mental distress.
Anxiety often becomes the dominant force during withdrawal – ironic since anxiety was likely what led to Valium use in the first place. This rebound anxiety can feel more severe than your original symptoms, creating panic about whether you’ll ever feel normal again. Depression may settle in like a heavy blanket, making simple tasks feel impossible.
Irritability becomes your default mode. Small annoyances that wouldn’t normally bother you – like traffic noise or someone chewing loudly – can trigger explosive anger. Your emotional regulation system is essentially offline, leaving you at the mercy of every feeling that surfaces.
Cognitive symptoms add another layer of difficulty. Brain fog makes concentration nearly impossible, while memory problems leave you forgetting conversations or losing track of simple tasks. Many people describe feeling detached from reality or experiencing a sense that nothing feels quite real.
Emotional and Mental Symptoms Include:
Severe anxiety and panic attacks
Depression and hopelessness
Irritability and mood swings
Difficulty concentrating
Memory problems
Feeling emotionally numb or detached
Increased sensitivity to stress
Severe Withdrawal Symptoms That Require Medical Attention
Some Valium withdrawal symptoms cross the line from uncomfortable to dangerous, requiring immediate professional intervention. Benzodiazepine withdrawal can be life-threatening, unlike withdrawal from many other substances, making medical supervision crucial for safety.
Seizures represent the most serious risk during diazepam withdrawal. These can occur without warning, especially in people who’ve used high doses or taken Valium for extended periods. Even if you’ve never had a seizure before, withdrawal can trigger them as your nervous system becomes hyperexcitable without the drug’s stabilizing effects.
Delirium tremens (DTs), while more commonly associated with alcohol withdrawal, can also occur during severe benzodiazepine withdrawal. This condition involves confusion, hallucinations, and dangerous changes in heart rate and blood pressure. Visual or auditory hallucinations may develop, creating terrifying experiences that feel completely real.
Extreme agitation or psychosis can emerge, particularly in people who developed benzodiazepine tolerance over months or years of use. Some individuals experience suicidal thoughts that feel overwhelming and persistent, making professional support essential for safety.
Warning Signs Requiring Emergency Care:
Any type of seizure activity
Hallucinations (visual, auditory, or tactile)
Severe confusion or disorientation
Chest pain or difficulty breathing
Extremely high blood pressure
Suicidal thoughts or behaviors
Inability to keep fluids down for extended periods
How Withdrawal Symptoms Differ Based on Usage Patterns
Your withdrawal experience depends heavily on how you’ve used Valium – the dose, duration, and frequency all play crucial roles in determining symptom severity and timeline. Understanding these patterns helps set realistic expectations and plan appropriate treatment approaches.
People who used high doses daily for months or years typically face the most challenging withdrawal. Their bodies have developed significant benzodiazepine tolerance, meaning their nervous systems have fundamentally changed to accommodate the drug’s presence. These individuals often need gradual dose reduction over many months to avoid severe complications.
Short-term users who took prescribed doses for a few weeks may experience milder symptoms, though withdrawal can still be uncomfortable. Their GABA receptors haven’t undergone as much adaptation, making the readjustment process shorter and less intense.
Withdrawal Patterns by Usage:
| Usage Pattern | Symptom Severity | Timeline | Special Considerations |
|---|---|---|---|
| Daily use 6+ months | Severe | Weeks to months | Requires medical tapering |
| Daily use 1-6 months | Moderate to severe | 1-4 weeks | Professional guidance recommended |
| As-needed use | Mild to moderate | Days to 2 weeks | May manage with support |
| High-dose abuse | Severe/dangerous | Extended timeline | Inpatient detox often necessary |
Valium addiction patterns also influence withdrawal difficulty. People who escalated their doses without medical supervision or mixed Valium with other substances face additional complications. Their withdrawal may include symptoms from multiple drug dependencies, requiring specialized diazepam detox treatment protocols.
Age and overall health status affect recovery speed and symptom intensity. Older adults often experience prolonged withdrawal symptoms, while underlying mental health conditions can complicate the emotional aspects of getting clean.
Valium Withdrawal Timeline and What to Expect
Acute Withdrawal Phase and Peak Symptom Period
The acute phase of Valium withdrawals typically begins within 1-4 days after your last dose, though this timing can vary based on individual factors. Unlike shorter-acting benzodiazepines, diazepam withdrawal often has a delayed onset due to its long half-life of 20-70 hours. This means the drug stays in your system longer, creating a buffer before withdrawal symptoms emerge.
Peak symptoms usually occur between days 7-14, when the most intense physical and psychological effects manifest. During this period, you might experience severe anxiety, panic attacks, muscle tension, tremors, and sleep disturbances. The GABA neurotransmitter system, which Valium has been artificially enhancing, struggles to function normally without the drug’s presence.
Common acute withdrawal symptoms include:
Physical symptoms: Sweating, nausea, headaches, muscle aches, trembling
Psychological symptoms: Intense anxiety, irritability, depression, confusion
Sensory disturbances: Heightened sensitivity to light, sound, and touch
Sleep issues: Insomnia, nightmares, restless sleep patterns
The acute phase typically lasts 2-8 weeks, gradually decreasing in intensity. However, some people experience waves of symptoms that come and go unpredictably during this time. Understanding that these symptoms are temporary and part of your body’s natural healing process can provide comfort during the most challenging days.
Protracted Withdrawal Syndrome and Long-Term Effects
Post-acute withdrawal symptoms (PAWS) can persist for months or even years after the acute phase ends. This protracted withdrawal syndrome affects approximately 10-25% of people recovering from benzodiazepine dependence. The symptoms are generally less severe than acute withdrawal but can be frustrating due to their unpredictable nature and extended duration.
Protracted symptoms often include:
Cognitive effects: Memory problems, concentration difficulties, brain fog
Emotional symptoms: Anxiety waves, depression, mood swings, emotional numbness
Physical manifestations: Fatigue, muscle tension, sleep disruption, digestive issues
Sensory sensitivities: Ongoing sensitivity to stimuli that gradually improves
The timeline for protracted withdrawal varies significantly. Some people notice improvement within 6-12 months, while others may experience lingering effects for 18-24 months or longer. The good news is that symptoms generally continue to improve over time, even if progress feels slow.
Your brain’s GABA receptors need time to heal and return to normal function after prolonged Valium use. This neurological recovery process happens gradually, which explains why protracted withdrawal can last so long. Supporting your nervous system through proper nutrition, stress management, and professional guidance can help speed this healing process.
Factors That Influence Your Personal Withdrawal Timeline
Your personal Valium withdrawal timeline depends on multiple interconnected factors that make each person’s experience unique. Understanding these variables can help set realistic expectations and guide your recovery planning.
Dosage and duration of use play the biggest role in determining withdrawal severity and length. Higher doses and longer periods of use typically lead to more intense and prolonged withdrawal symptoms. Someone taking therapeutic doses for a few months will likely have a different experience than someone who has used high doses for several years.
Individual biological factors significantly impact your withdrawal journey:
| Factor | Impact on Withdrawal |
|---|---|
| Age | Older adults often experience longer withdrawal periods |
| Metabolism | Slower metabolism can extend withdrawal timeline |
| Overall health | Better physical health supports faster recovery |
| Genetics | Some people naturally process medications differently |
| Mental health history | Pre-existing conditions can complicate withdrawal |
Tapering approach dramatically affects your experience. Rapid discontinuation or “cold turkey” withdrawal typically causes more severe symptoms and potential complications. A gradual dose reduction over weeks or months allows your brain time to adjust, resulting in a more manageable withdrawal process.
Lifestyle factors also influence your recovery timeline. Regular exercise, proper nutrition, adequate sleep, and stress management all support your nervous system’s healing process. Conversely, high stress levels, poor sleep habits, and substance use can prolong withdrawal symptoms.
The presence of other medications or substances can interact with your withdrawal process. Some medications may help ease symptoms, while others might complicate recovery. Always work with healthcare professionals who understand benzodiazepine withdrawal to navigate these complexities safely.
Safe Medical Detox and Tapering Strategies

Why Professional Medical Supervision Is Essential
Valium withdrawals can turn dangerous fast, especially for people who’ve been taking higher doses or using the medication for extended periods. Medical professionals understand how benzodiazepine withdrawal affects your GABA neurotransmitter system and can spot warning signs that most people miss.
Professional detox Valium programs monitor your vital signs around the clock, watching for seizures, severe anxiety spikes, and cardiovascular complications. These medical teams know exactly when to adjust your tapering schedule or introduce supportive medications to keep you safe.
Trying to quit cold turkey or managing withdrawal alone puts you at serious risk. Medical supervision provides the safety net you need during this vulnerable time, with trained staff who can respond immediately if complications arise.
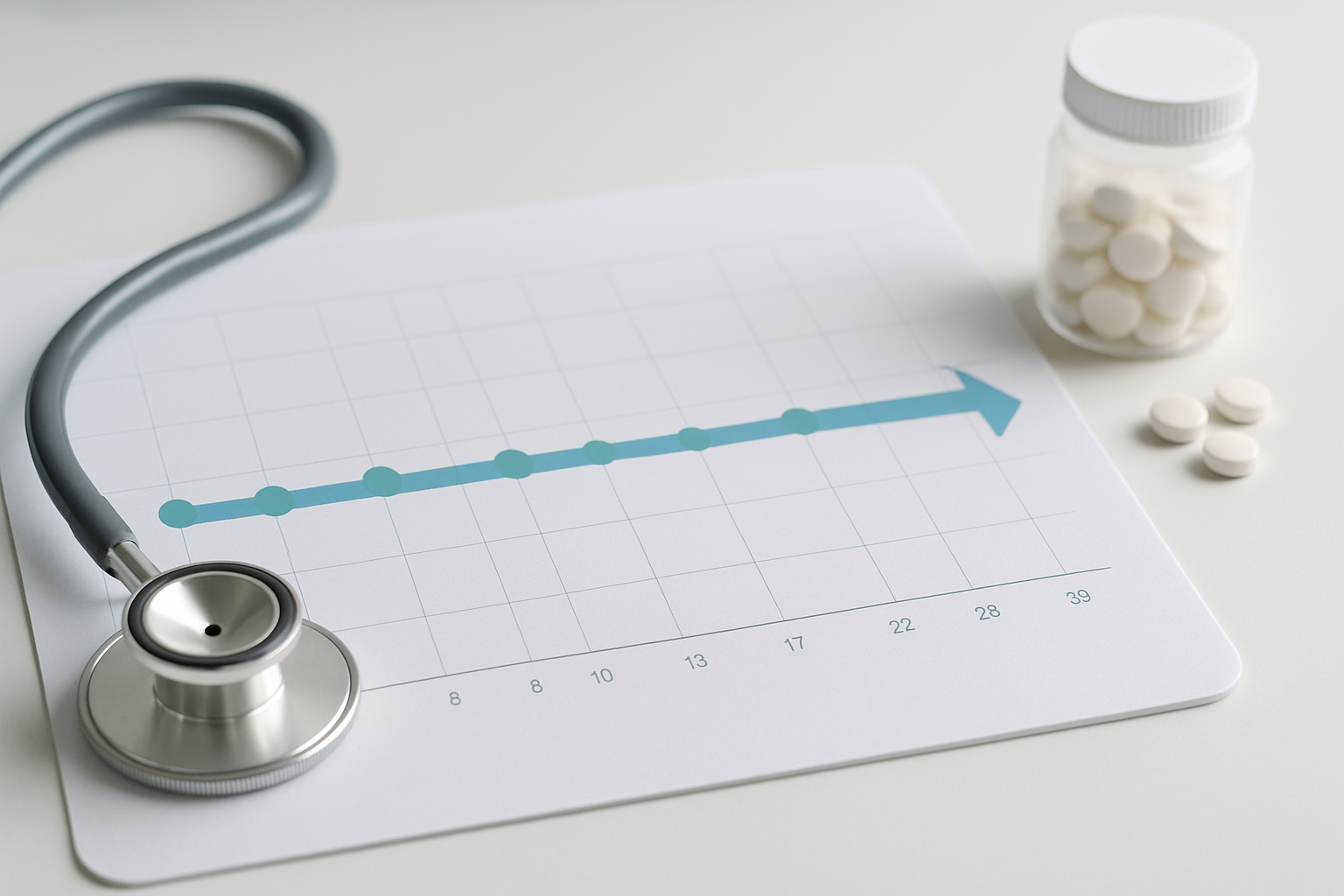
Gradual Tapering Schedules That Minimize Discomfort
Gradual dose reduction Valium represents the gold standard for safe withdrawal. Most medical professionals recommend reducing your daily dose by 10-25% every 1-2 weeks, depending on how long you’ve been taking the medication and your current dosage.
Here’s what a typical tapering schedule might look like:
| Week | Daily Dose Reduction | Symptoms to Monitor |
|---|---|---|
| 1-2 | 25% reduction | Sleep disruption, mild anxiety |
| 3-4 | 15% reduction | Increased anxiety, irritability |
| 5-6 | 10% reduction | Physical discomfort, mood changes |
| 7-8 | 10% reduction | Concentration issues, fatigue |
Some people need slower tapers, especially those who’ve used Valium for months or years. Your medical team might stretch this process over several months, making smaller reductions to minimize acute withdrawal symptoms Valium.
The key is flexibility – your taper should adjust based on how your body responds. If you’re experiencing severe discomfort, your doctor might slow down the process or temporarily stabilize you at your current dose.
Medications That Help Manage Withdrawal Symptoms
Several medications can ease the discomfort of diazepam withdrawal without creating new dependencies. Anti-seizure medications like gabapentin often help with anxiety and sleep problems during tapering Valium withdrawal.
Beta-blockers such as propranolol can manage physical symptoms like rapid heartbeat, tremors, and high blood pressure. These medications target the body’s stress response without interfering with your brain’s healing process.
For sleep issues, doctors might prescribe non-habit-forming options like trazodone or melatonin. Some facilities use clonidine to help with autonomic nervous system symptoms like sweating, nausea, and temperature regulation problems.
Antidepressants sometimes play a role in longer-term recovery, especially for people dealing with underlying anxiety or depression that initially led to Valium use.
When Inpatient Treatment Becomes Necessary
Inpatient diazepam detox treatment becomes essential when outpatient tapering isn’t working or when you’re at high risk for complications. People taking large daily doses (above 40mg) often need residential supervision during the initial withdrawal phase.
Medical history plays a huge role in this decision. If you have a history of seizures, heart problems, or previous difficult withdrawals from benzodiazepines, inpatient care provides the intensive monitoring you need.
Psychological factors matter too. Severe anxiety, panic disorders, or concurrent mental health conditions often require the structured environment and immediate support that residential facilities provide.
Inpatient programs typically last 5-14 days for the acute phase, followed by outpatient support for continued tapering. These facilities combine medical supervision with counseling and education about Valium addiction treatment, giving you tools for long-term recovery success.
Natural Support Methods During Withdrawal

Nutritional Support and Supplements That Aid Recovery
Your body works overtime during Valium withdrawals, burning through essential nutrients while your system rebalances itself. Proper nutrition becomes your foundation for healing, helping reduce withdrawal symptoms and supporting your brain’s natural recovery process.
Essential Nutrients for Recovery:
Magnesium (400-600mg daily) helps calm the nervous system and reduces muscle tension, anxiety, and insomnia commonly experienced during benzodiazepine withdrawal
B-Complex vitamins support neurotransmitter production and energy metabolism, particularly B1, B6, and B12 which are often depleted during chronic Valium use
Omega-3 fatty acids (2-3g daily) reduce brain inflammation and support GABA neurotransmitter function
Vitamin D deficiency worsens anxiety and depression symptoms, making supplementation crucial
GABA supplements may provide mild calming effects, though they don’t cross the blood-brain barrier as effectively as medications
Recovery-Supporting Foods:
| Food Category | Examples | Benefits |
|---|---|---|
| Complex Carbs | Quinoa, brown rice, sweet potatoes | Stabilize blood sugar and mood |
| Lean Proteins | Fish, chicken, legumes | Support neurotransmitter production |
| Healthy Fats | Avocados, nuts, olive oil | Reduce inflammation |
| Antioxidant-rich | Berries, leafy greens, dark chocolate | Protect brain cells |
Avoid caffeine, alcohol, and processed sugars, as these can worsen anxiety and disrupt sleep patterns during your recovery.
Exercise and Physical Activities That Reduce Symptoms
Physical activity becomes a powerful ally during Valium detox, naturally boosting endorphins and helping your body process stress hormones more effectively. Exercise also improves sleep quality and reduces the intensity of physical withdrawal symptoms.
Low-Impact Activities for Early Withdrawal:
Walking for 20-30 minutes daily helps reduce anxiety without overwhelming your system
Gentle yoga combines movement with breathing exercises, addressing both physical tension and mental stress
Swimming provides full-body exercise while being easy on joints and promoting relaxation
Tai Chi offers slow, meditative movements that improve balance and reduce anxiety
Building Exercise Tolerance:
Start with just 10-15 minutes of gentle activity and gradually increase duration as your energy returns. Your cardiovascular system may be sensitive during early withdrawal, so listen to your body and avoid pushing too hard.
Strength Training Benefits:
Once past acute withdrawal symptoms, light resistance training helps rebuild muscle tone and improves mood through endorphin release. Focus on bodyweight exercises like modified push-ups, wall sits, and resistance band work.
Remember that consistency matters more than intensity. A daily 15-minute walk does more for your recovery than sporadic intense workouts that leave you exhausted.
Stress Management Techniques for Emotional Stability
Psychological withdrawal from Valium often includes heightened anxiety, mood swings, and emotional sensitivity. Learning healthy stress management techniques helps you navigate these challenges without relying on medications.
Breathing Techniques:
4-7-8 breathing: Inhale for 4 counts, hold for 7, exhale for 8. This activates your parasympathetic nervous system
Box breathing: Equal counts for inhale, hold, exhale, hold (try 4-4-4-4 initially)
Diaphragmatic breathing helps counteract the shallow breathing patterns common during anxiety
Mindfulness Practices:
Daily meditation, even for 5-10 minutes, helps rewire your brain’s response to stress. Apps like Headspace or Calm provide guided sessions specifically designed for anxiety management.
Progressive Muscle Relaxation:
This technique involves tensing and releasing muscle groups systematically, helping you recognize and release physical tension that accompanies emotional stress.
Cognitive Strategies:
Grounding techniques (5-4-3-2-1 method: name 5 things you see, 4 you hear, 3 you feel, 2 you smell, 1 you taste)
Journaling helps process emotions and track progress
Positive self-talk replaces catastrophic thinking patterns
Sleep Hygiene Practices for Better Rest During Withdrawal
Sleep disturbances rank among the most challenging aspects of Valium withdrawals. Since diazepam affects GABA receptors that regulate sleep, your natural sleep patterns need time to reestablish themselves.
Creating Your Sleep Environment:
Keep your bedroom between 65-68°F
Use blackout curtains or eye masks to block light
Remove electronic devices at least 1 hour before bed
Consider white noise machines or earplugs for sound control
Pre-Sleep Routine:
Develop a consistent routine starting 1-2 hours before bedtime:
Warm bath or shower with Epsom salts (magnesium absorption through skin)
Herbal tea like chamomile, passionflower, or valerian root
Gentle stretching or light yoga poses
Reading (physical books, not screens) or listening to calming music
Meditation or prayer for mental preparation
Managing Sleep Anxiety:
Accept that sleep may be difficult initially – anxiety about not sleeping makes insomnia worse
Use the “20-minute rule”: If you can’t fall asleep within 20 minutes, get up and do a quiet activity until sleepy
Practice sleep restriction therapy: limit time in bed to actual sleep time, gradually increasing as sleep improves
Natural Sleep Aids:
Melatonin (0.5-3mg) taken 30 minutes before desired bedtime
L-theanine (100-200mg) promotes relaxation without sedation
Magnesium glycinate (200-400mg) before bed supports muscle relaxation
Avoid relying on other sleep medications during Valium withdrawal, as this can interfere with your brain’s natural rebalancing process and potentially create new dependencies.
Building Long-Term Recovery Success

Therapy Options That Address Underlying Issues
Successful recovery from Valium withdrawals goes beyond just managing physical symptoms. Most people who develop benzodiazepine dependence have underlying mental health conditions like anxiety, panic disorders, or trauma that led them to use Valium in the first place. Cognitive Behavioral Therapy (CBT) stands out as one of the most effective approaches, helping you identify negative thought patterns and develop healthier coping mechanisms without relying on medication.
Trauma-informed therapy becomes essential if your Valium use started as a way to numb emotional pain or manage PTSD symptoms. EMDR (Eye Movement Desensitization and Reprocessing) and somatic experiencing can help process traumatic memories that might trigger cravings during recovery. Many people find that addressing these root causes prevents the cycle of returning to Valium when life gets stressful.
Dialectical Behavior Therapy (DBT) offers powerful tools for managing intense emotions and building distress tolerance skills. These techniques become invaluable when facing post-acute withdrawal symptoms or life challenges that previously would have sent you reaching for your pill bottle. Group therapy sessions create connections with others who understand the unique struggles of benzodiazepine withdrawal, reducing isolation and shame.
Some treatment centers now offer specialized programs specifically for benzodiazepine addiction, recognizing that benzo withdrawals require different approaches than other substance dependencies. These programs combine medical supervision with psychological interventions tailored to the specific challenges of GABA neurotransmitter recovery.
Support Systems and Resources for Ongoing Recovery
Building a strong support network becomes your lifeline during long-term recovery from Valium addiction. Family and friends often struggle to understand the prolonged nature of benzodiazepine withdrawal, so education becomes key. Sharing resources about post-acute withdrawal symptoms helps loved ones recognize that your recovery journey extends far beyond the initial detox phase.
Peer support groups specifically for benzodiazepine recovery offer unique understanding that general addiction meetings might not provide. The Benzodiazepine Information Coalition and online communities like BenzoBuddies connect you with people who truly get the extended timeline and complex symptoms of benzo withdrawals. These connections provide hope during difficult moments and practical strategies from those further along in recovery.
Professional support teams should include addiction counselors familiar with benzodiazepine dependence, psychiatrists experienced in gradual dose reduction protocols, and primary care physicians monitoring your overall health. Regular check-ins with these professionals help adjust your recovery plan as needed and address emerging challenges before they become overwhelming.
Recovery coaching offers personalized guidance for navigating daily life challenges without Valium. These professionals help you develop practical strategies for managing work stress, relationship conflicts, and health concerns that might previously have triggered medication use. Many insurance plans now cover these services, making professional support more accessible.
| Support Type | Benefits | How to Access |
|---|---|---|
| Peer Support Groups | Shared understanding, practical tips | BenzoBuddies, local addiction centers |
| Professional Counseling | Expert guidance, trauma processing | Insurance, sliding scale fees |
| Family Education | Improved relationships, better support | Family therapy, educational resources |
| Recovery Coaching | Daily life strategies, accountability | Private practice, treatment centers |
Preventing Relapse and Managing Triggers
Relapse prevention starts with identifying your personal triggers for Valium use. Common triggers include medical procedures, job stress, relationship conflicts, insomnia, and anniversary dates of traumatic events. Creating a detailed trigger map helps you prepare specific responses for high-risk situations before they arise.
Developing a comprehensive relapse prevention plan includes emergency contacts, coping strategies, and clear steps to take if cravings become overwhelming. This plan should list specific people to call, grounding techniques that work for you, and safe spaces where you can ride out difficult moments. Keep copies in multiple locations and share with trusted support people.
Stress management techniques become essential life skills during recovery. Regular exercise helps restore natural GABA production and reduces anxiety without medication. Meditation, yoga, and breathing exercises provide immediate tools for managing panic symptoms that might otherwise trigger Valium cravings. Progressive muscle relaxation can be particularly helpful for those experiencing ongoing physical tension from withdrawal.
Sleep hygiene deserves special attention since insomnia often drives people back to benzodiazepines. Establishing consistent bedtime routines, limiting screen time, and creating a comfortable sleep environment support natural sleep cycles. Some people benefit from magnesium supplements or melatonin, but always discuss these with your healthcare team first.
Building new routines that don’t involve medication creates positive momentum in recovery. This might include morning walks, creative hobbies, volunteer work, or learning new skills. These activities provide natural mood boosts and sense of accomplishment that medication once provided artificially.
Environmental changes sometimes become necessary for successful recovery. This could mean avoiding certain social situations temporarily, changing doctors who over-prescribe medications, or removing pills from easy access. Some people find that changing their living situation helps break old patterns associated with Valium use.
7 FAQ

How long do Valium withdrawals last?
Valium withdrawal symptoms typically begin 1-4 days after stopping and can last several weeks to months. Acute withdrawal peaks around day 7-14, lasting 2-4 weeks. Post-acute withdrawal syndrome may persist for months, with symptoms gradually improving. The extended timeline reflects diazepam’s long half-life and depends on factors like dosage, duration of use, and individual metabolism.
What are the most dangerous Valium withdrawal symptoms?
Seizures pose the greatest risk during Valium withdrawal, especially with abrupt discontinuation or high-dose dependence. Other serious symptoms include severe anxiety, panic attacks, delirium tremens, and cardiovascular complications. Psychological symptoms like depression and suicidal thoughts also require immediate attention. Medical supervision prevents life-threatening complications through proper tapering and monitoring.
Can I detox from Valium at home?
Home detox from Valium carries significant risks and isn’t recommended for heavy users or those with medical conditions. The seizure risk makes professional supervision essential. If attempting gradual tapering at home, work closely with a doctor who can monitor progress and adjust dosing. Medical detox facilities provide 24/7 monitoring and emergency intervention when needed.
What medications help with Valium withdrawal?
Doctors may prescribe longer-acting benzodiazepines like chlordiazepoxide for gradual tapering. Anticonvulsants such as carbamazepine help prevent seizures. Beta-blockers manage heart rate and blood pressure. Antidepressants address mood symptoms. Sleep aids and anti-nausea medications provide symptomatic relief. All medications require medical supervision to prevent interactions and ensure safety.
How do I know if I’m physically dependent on Valium?
Physical dependence develops when your body requires Valium to function normally. Signs include needing higher doses for the same effect (tolerance), experiencing withdrawal symptoms when stopping, and taking Valium to avoid discomfort rather than for therapeutic benefits. Even prescribed users can develop dependence within weeks of regular use.
What’s the difference between Valium addiction and dependence?
Physical dependence involves bodily adaptation to Valium, causing withdrawal when stopped. Addiction includes psychological compulsion, continued use despite harm, and loss of control. Someone can be dependent without being addicted (prescribed users) or addicted without severe physical dependence. Both conditions require professional treatment but use different approaches.
Are there natural ways to ease Valium withdrawal symptoms?
Natural support methods complement medical treatment but shouldn’t replace professional care. Regular exercise releases endorphins and reduces anxiety. Meditation and deep breathing calm the nervous system. Nutritional support with B-vitamins, magnesium, and omega-3s helps restore brain chemistry. Herbal teas like chamomile provide mild relaxation. Always consult doctors before combining natural methods with medications.

Valium withdrawal doesn’t have to be something you face alone or without proper support. The symptoms can feel overwhelming, but understanding what’s happening in your body and having a clear timeline helps you prepare mentally and physically for the journey ahead. Medical detox and gradual tapering remain the safest approaches, giving your brain the time it needs to readjust naturally while minimizing dangerous complications.
Recovery extends far beyond just getting through the withdrawal phase. Combining professional medical care with natural support methods like proper nutrition, gentle exercise, and stress management creates a solid foundation for healing. Building healthy coping strategies and connecting with support systems early on sets you up for lasting success. If you’re considering stopping Valium, reach out to a healthcare professional who can create a personalized withdrawal plan that keeps you safe and comfortable throughout the process.
Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals| Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals | Valium withdrawals
